How should women with PAS be cared for?
Placenta Accreta Ireland work in close collaboration with healthcare providers who look after women with PAS in Ireland. The information provided here about the care of women with PAS will be most relevant to women and their families who are being cared for in Ireland.
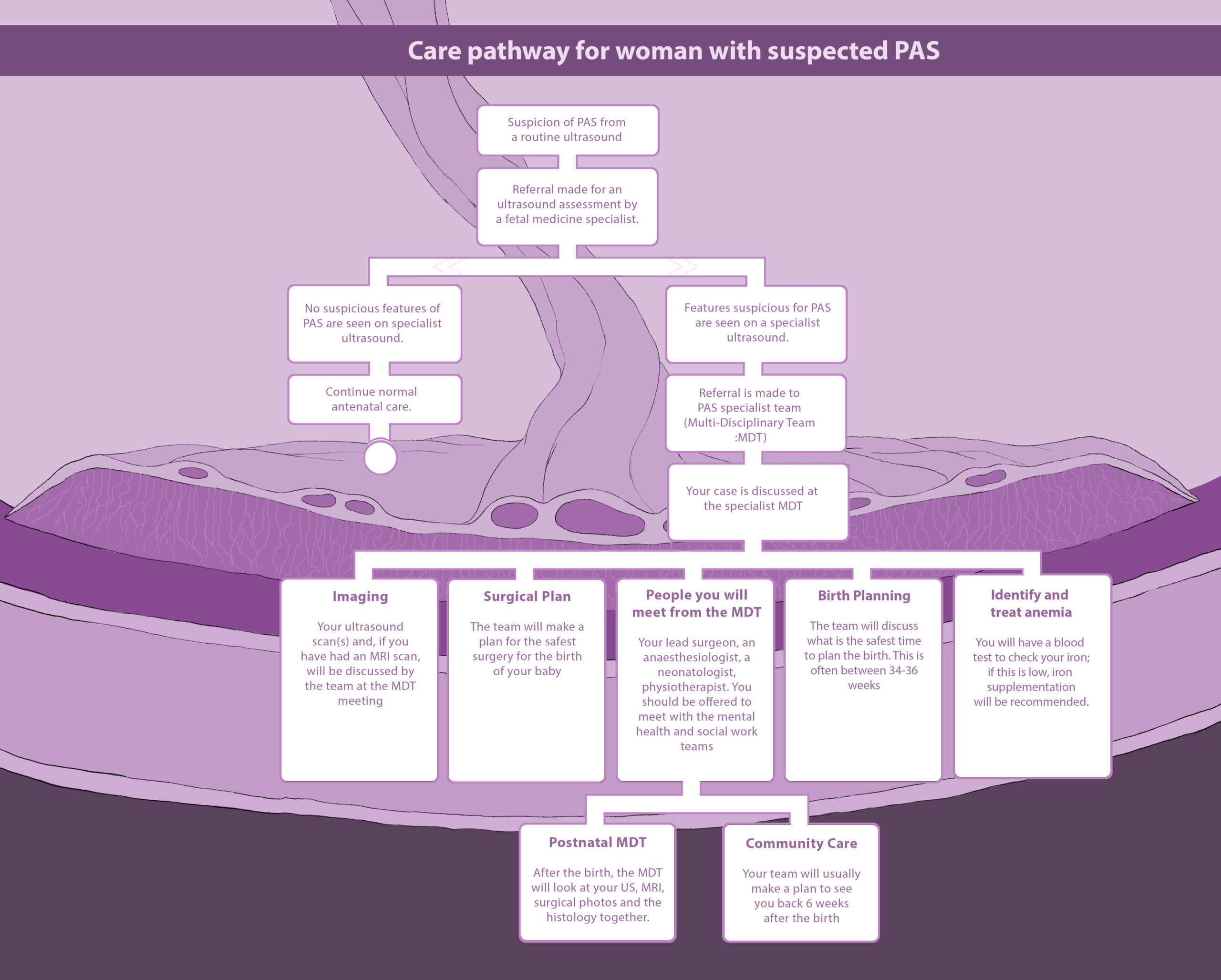
Women with placenta accreta spectrum should have the opportunity to meet members of the team at various times during the pregnancy.
If you are being looked after by a specialist team, at a regular multidisciplinary meeting, members of the team will meet to make a plan for your pregnancy and birth. A scheduled or planned delivery is safest for you and your baby. If there is any heavy bleeding or concerns about the health of the mother or baby an emergency delivery may need to be performed.





Place of care
Some women with placenta accreta will need to be admitted to the hospital. This may happen if they have any bleeding or pain during your pregnancy or if they live a long way from the hospital. Most women with placenta accreta spectrum will not need to be admitted to hospital, and can safely be cared for while at home. Usually, ultrasound scans with the specialist team will be performed every 2-4 weeks. Women should still go to their routine antenatal care to have the usual tests performed during pregnancy, such as blood pressure, checked regularly.
Birth planning
Women with placenta accreta spectrum will need to give birth by caesarean section. The safest type of birth for women and their baby is an elective (planned) birth. For that reason, the team will usually make a plan to give birth a few weeks before the due date, often between 34-36 weeks. This reduces the chance that women will have bleeding or go into labour and need an emergency birth. If the baby is delivered before 34 weeks, two steroid injections will be given to the mother to help the babies lung development.
Anaesthesia for the birth
For a caesarean birth for women with placenta accreta spectrum, it can be helpful to think of the procedure in two parts – “the birth” and “the surgery”. The first part is from the start of the caesarean birth until the baby is born, which may take between 1 to 1.5 hours. The second part is after the baby is born and the surgical team will take time to perform rest of the surgery. This can often take another 1 to 2 hours. The time the second part of the operation takes will vary and depends on many factors such as if a hysterectomy is planned (removal of the womb) or if any complications occur.
Combined Spinal- Epidural Anaesthesia: Combined spinal- epidural anaesthesia is a regional anaesthetic technique that is routinely used for planned caesarean births. It is a safe and effective anaesthetic that allows women to be awake and pain free during the birth of their baby. A combined spinal- epidural anaesthetic is a single injection of local anaesthetic medication given into the lower back. The nerves are blocked and this means women will be numb from the top of the chest down to the feet. This is the most common form of anaesthesia for planned caesarean births. Following this injection of local anaesthesia medication, a very fine catheter (tube) is placed in the epidural space. This catheter allows for local anaesthetic medication to be given continuously, providing excellent pain relief for hours or days after the birth, as needed.
General Anaesthesia: Following delivery of the baby, general anaesthesia can be used while the obstetricians and theatre team undertake any other necessary actions. General anaesthesia can also be used in the event that a combined spinal-epidural anaesthesia technique is not possible, e.g. due to disorders of blood clotting, haemorrhage, or when an urgent caesarean birth is required and there is not enough time to establish a regional anaesthetic.
Some women may need an emergency caesarean birth and the situation will determine the safest type of anaesthetic. The priority is to make sure that the safest approach is taken for each woman’s unique situation.
Surgery for the birth
The type of surgery need to treat placenta accreta spectrum will be different for each woman. The most suitable treatment for each women will be decided at the multi-disciplinary team. The team will take into account the ultrasound and MRI findings, as well as the woman’s medical history and her preferences.
Surgical incision: some women will need a vertical (up and down) incision on the abdomen. This means you will have a scar which goes from the pubic bone to above your belly button. For other women, they will have an incision similar to a normal caesarean birth, a transverse (across) incision between the hip bones.
Uterine conserving surgery: “Uterine conserving surgery” means that a hysterectomy is not performed by the medical team. Carefully selected women will be suitable for this type of treatment. The specialist team will have looked at the ultrasound and MRI images and may decide this is a suitable option. Sometimes, there may have been a plan to go ahead with a hysterectomy, but when the surgical team examine the womb and placenta at the time of surgery, they will find only a small part of the placenta is attached to the lining of the womb. In these cases, uterine conserving surgery will also be suitable.
Uterine conserving surgery is performed by “myometrial resection”. This means only a small part of the womb is removed, along with the placenta. The womb is then sutured back together and will heal over the weeks and months after the birth, similar to having a routine caesarean section.
Caesarean hysterectomy: Hysterectomy means removal of the womb, along with the placenta, after the baby is born. This may be planned or happen in an emergency because of heavy bleeding. When the ultrasound and MRI images show there is severe placenta accreta spectrum (grade 3), the specialist team may make a plan for hysterectomy. In other cases, uterine conservation may have been planned, however when the medical team examine the womb and placenta at the time of surgery, a hysterectomy is performed because they find severe placenta accreta spectrum.
Fallopian tubes and ovaries: When women have a hysterectomy, the fallopian tubes are usually removed at the same time. This is because removal of the fallopian tubes reduces the risk of getting ovarian cancer later in life. If women are having uterine conserving surgery and their family is finished, they can choose to have the fallopian tubes removed at the time of the birth also. The ovaries will not be removed, and will continue to make important hormones until the time of the menopause.
Aortic balloon: For some women, an aortic balloon will be inserted to reduce the risk of bleeding during the surgery. A specialist X-ray doctor inserts a balloon into a large blood vessel (the aorta) which brings blood to the lower half of the body, including the womb. This reduces the risk of heavy bleeding during the birth and surgery. The balloon is inserted through a small incision in the groin. The medical team will inflate the balloon during the surgery for a few minutes at a time after the baby has been born. The balloon is removed at the end of the surgery. This is only performed in select cases and a decision is made on a case by case basis by the specialist team.
Content prepared by: Dr Helena Bartels & Prof Donal Brennan, Placenta Accreta Service
Date posted: January 2023
Date last review: February 2023

