What is Placenta Accreta Spectrum?
Placenta Accreta Ireland work in close collaboration with healthcare providers who look after women with PAS in Ireland. The information provided here about the care of women with PAS will be most relevant to women and their families who are being cared for in Ireland.
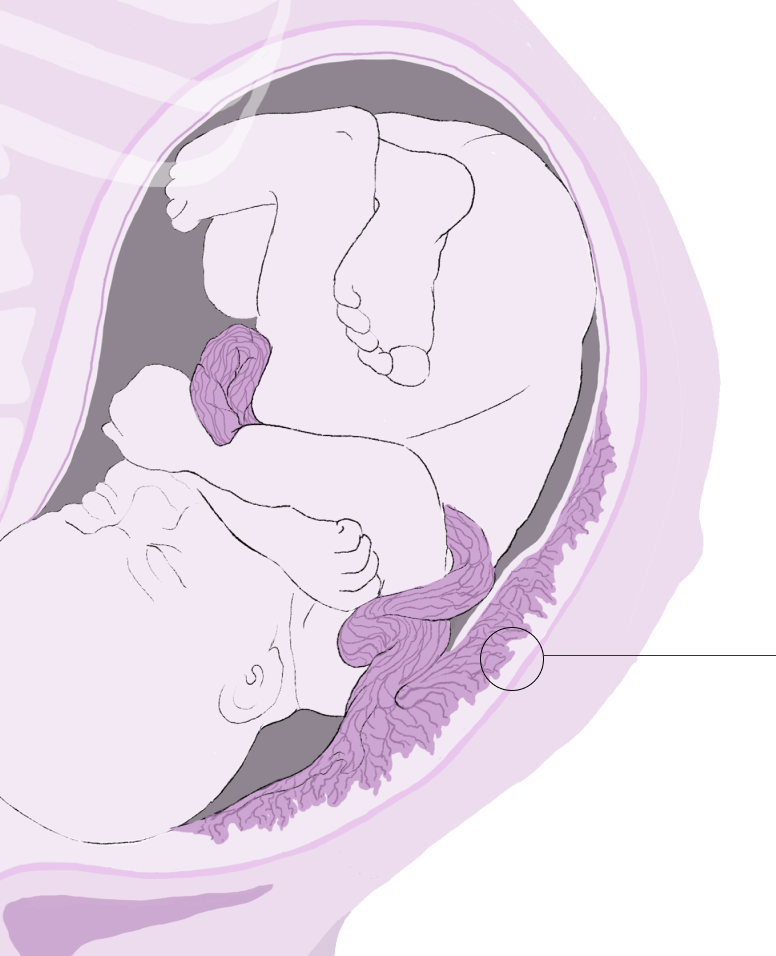
“Placenta accreta spectrum” covers a range of clinical conditions where the placenta is abnormally attached to the lining of the womb. The placenta is a temporary organ that connects the unborn baby to the wall of the womb through the umbilical cord. The placenta gives oxygen and nutrients to the baby during pregnancy. Usually, the placenta will separate from the lining of the womb after the baby is born.
In cases of placenta accreta spectrum, the placenta is abnormally attached to the lining of the womb and does not separate after the birth. The condition is a rare complication of pregnancy. However, because of many factors such as more women giving birth by caesarean section and using fertility treatments to get pregnant, placenta accreta is becoming more common.
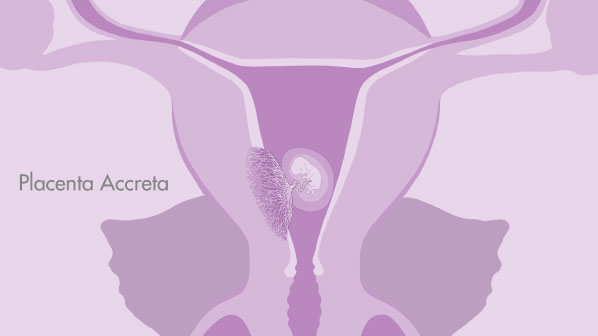
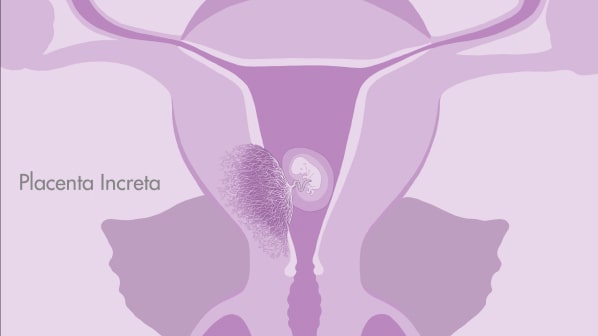
Placenta accreta spectrum is divided into “placenta accreta” and “placenta increta”. In placenta accreta, the placenta is abnormally attached to the muscle of the womb, which is called the myometrium. In placenta increta, the placenta is grown more deeply into the myometrium than in placenta accreta. In both conditions, the placenta will not separate from the womb after the birth, and stays stuck to the muscle of the womb.
What are the risk factors for developing PAS?
Placenta accreta spectrum is more likely to happen if:
It is important to remember that most women who have these risk factors will not develop placenta accreta spectrum. However, they put you at higher risk of developing the condition.
How is PAS diagnosed?
Placenta accreta spectrum is suspected during pregnancy on an ultrasound scan. Ultrasound signs of placenta accreta spectrum are looked for by a specialist doctor or sonographer, usually in women who have risk factors. If there are ultrasound signs of placenta accreta spectrum, regular ultrasound scans will be performed during the pregnancy to look closely at the placenta as the pregnancy progresses. While it is possible to diagnose the condition at any stage during pregnancy, usually the first signs are not seen until the 20 – 22 week anatomy ultrasound. In many cases the ultrasound features may not become clear until later in pregnancy around 28 weeks.
For some women, an MRI scan is arranged. MRI uses a strong magnetic field and radio waves to make detailed images of the organs and tissues in the body. While ultrasound is the best test to look at the placenta itself, an MRI allows the team of doctors to see if other organs close to the womb, such as the bladder are involved. The team of doctors will use both the ultrasound and MRI images together to see how deeply the placenta may be attached to the lining of the womb. Both ultrasound and MRI are safe during pregnancy and do not harm cause harm to the baby.
Most women with placenta accreta spectrum will not have any symptoms. Some women may have bleeding from the placenta.
Content prepared by: Dr Helena Bartels & Prof Donal Brennan, Placenta Accreta Service
Date posted: January 2023
Date last review: February 2023

