What is a Caesarean scar pregnancy?
How is a Caesarean scar pregnancy diagnosed?
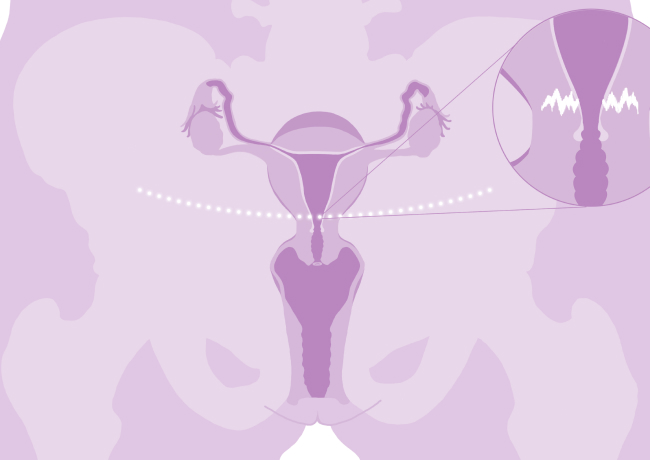
- CSP is diagnosed by an ultrasound scan. An ultrasound scan is a procedure that uses sound waves to produce images of certain parts of the body.
- Usually, an abdominal ultrasound and a transvaginal ultrasound (internal scan) are performed to make the diagnosis. In the early weeks of the pregnancy, the internal (transvaginal) scan is more accurate than the transabdominal one. This scan is usually performed in a maternity hospital, by a specialised practitioner in pregnancy ultrasound.
- Typical signs for CSP are looked for when you are having a scan.
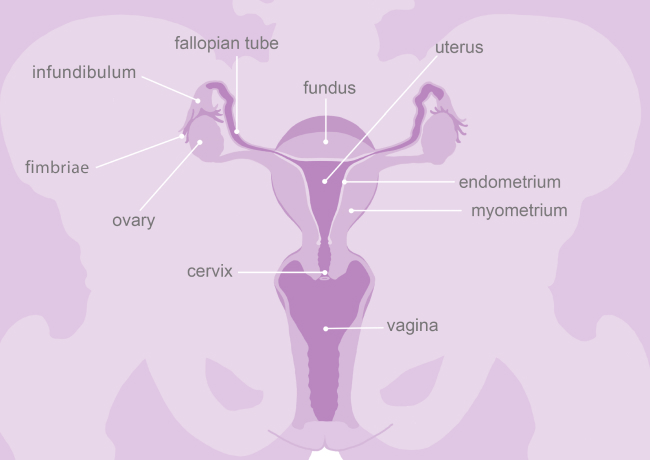
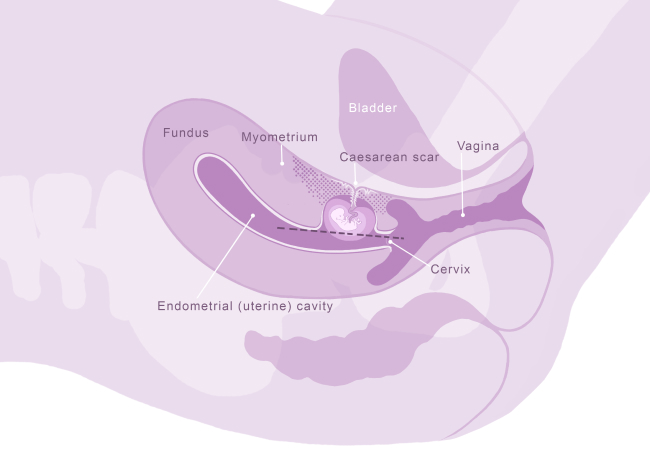
- These signs include a pregnancy which is low down in the womb and is located over or within the previous Caesarean scar.
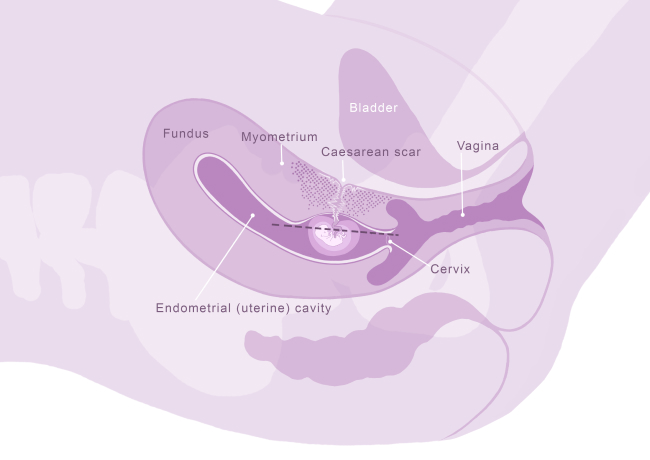
- There are different types of CSP. Generally, these can be divided into two types.
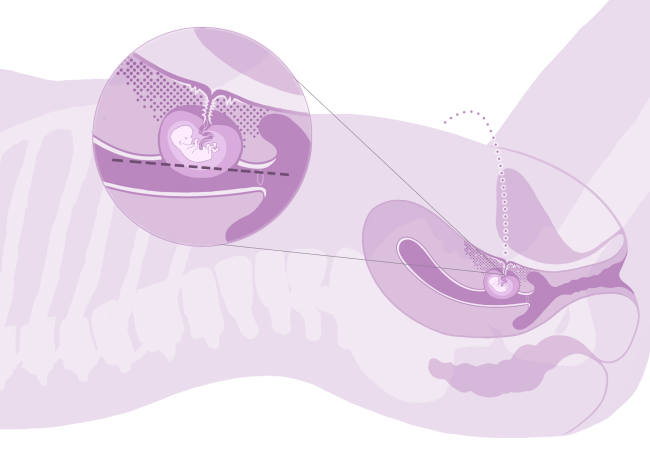
- In a type 1 CSP, the pregnancy is located over the old Caesarean scar and appears to be growing towards the top cavity (fundus) of the womb.
- In a type 2 CSP, the pregnancy is located within the old Caesarean scar, and is growing more towards the bladder. This a more severe form with more risks for mother and baby. These risks are discussed in more detail below.
What are the risks associated with Caesarean scar pregnancy?
- Bleeding complications. Women are at risk of bleeding in pregnancy and during labour and delivery and even during surgical treatment of CSP. In case of life-threatening bleeding women may need a blood transfusion and possibly a life-saving hysterectomy (removal of the womb).
- CSP can develop into one of the forms of adherent placenta called “placenta accreta spectrum”: if the pregnancy continues into the 2nd and 3rd trimester, some women with CSP will develop placenta accreta spectrum. This is more likely if the CSP is a type 2 CSP as described above, however it can happen with all types of CSP. To read more about the risks of placenta accreta spectrum, please refer to the section about placenta accreta spectrum (placenta accreta spectrum).
- Rupture of the womb: this means the pregnancy grows through the previous Caesarean scar and creates an opening through the wall of the womb (uterus). This complications is rare but can be life threatening. It can occur in all three trimesters of the pregnancy and some studies have reported that up to 1 in 10 women with CSP may have a uterine rupture after 12 weeks.
- Complications of treatment: women having treatment for CSP, such as surgery or medical treatment, may have complications as a result of this (see below for further details).
What you can expect when a Caesarean scar pregnancy is diagnosed?
- Your doctor will explain the diagnosis, and in some cases, will refer you to a specialist hospital to have another scan with a specialist practitioner. As CSPs are very rare, not all hospitals will have the expertise to diagnose and care for women with this condition.
- Your doctor will discuss your scan findings with you, and talk to you about the plan for your care and pregnancy.
- There are a number of serious risks for the mother and baby when a CSP is diagnosed. Your doctor will discuss these with you. These risks depend on:
- How many weeks pregnant you are
- What type of CSP is diagnosed (type 1 or type 2)
- If you have symptoms such as pain or bleeding
- If the pregnancy is viable (there is a heartbeat present)
- Your medical and surgical history
How is a Caesarean scar pregnancy managed?
There are a number of different ways a CSP can be managed. This depends on the type of CSP and at how many weeks the diagnosis is made, as well as the mothers preferences. There is no best practice or “one size fits all” approach on how to manage CSP. This condition is rare and each case will need special planning by your medical team, taking into account all of the specific details of the pregnancy, the ultrasound findings and the informed woman’s choice.
There are two main treatment routes for CSP: ending the pregnancy (termination) or trying to continue the pregnancy into the 3rd trimester of pregnancy (expectant management). Making a decision soon after the diagnosis of CSP is made is important. This is especially the case for women who are ending the pregnancy since with every day the pregnancy grows, the risk of complications increases. Below, the two management routes are discussed in more detail.
Management
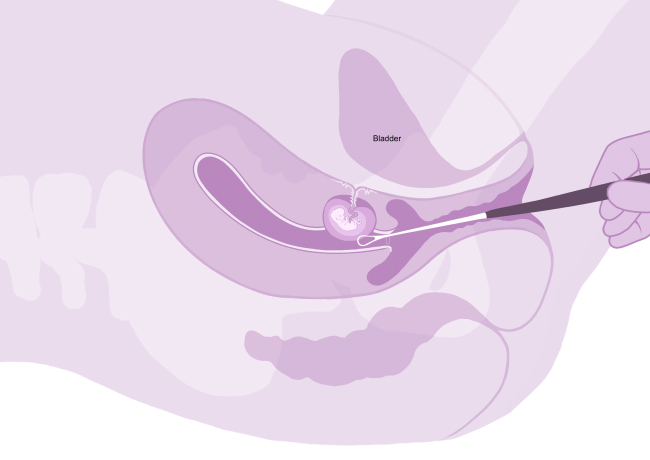
- bleeding requiring a blood transfusion
- hysterectomy (removal of the womb)
- uterine perforation (the doctor making a hole in the womb during the surgery)
- haematoma formation (blood clot in the womb which may take weeks to months to resolve. In some cases, this may need further surgery if it does not resolve and is causing symptoms such as pain and irregular bleeding)
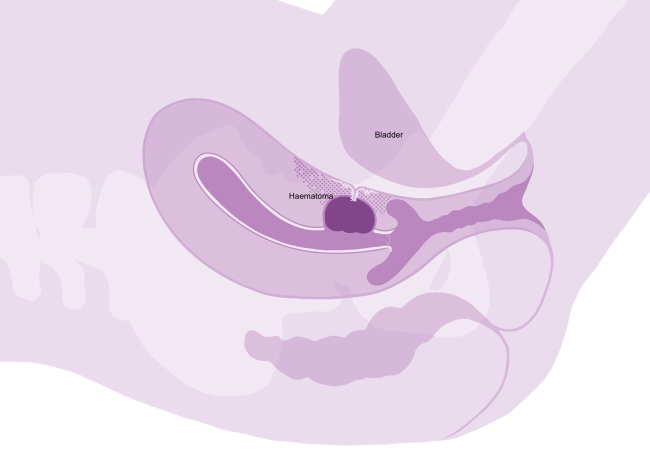

- bleeding requiring a blood transfusion
- hysterectomy (removal of the womb). This may be needed if there is very heavy bleeding, or if there is a very complicated or big hole (defect) in the womb
- This means taking medication, usually to make the womb contract, to end the pregnancy.
- This may be recommended if there is no fetal heartbeat and the pregnancy is measuring small or very early in the pregnancy, and on ultrasound it looks like a type 1 CSP.
- This means continuing the pregnancy in the hope of having a healthy baby.
- If there is a fetal heartbeat present, you will be counselled on your options of treatment.
- Some women in this scenario, where there is a fetal heartbeat present, may decide to continue the pregnancy in the hope of having a healthy baby.
- The means the pregnancy keeps growing and, in some cases, may continue to the third trimester.
- The risks are as described above, such as life threatening rupture of the womb or developing placenta accreta spectrum later in the pregnancy.
- Although this is high risk, many women who choose this option go on to have a baby.
- As described above, there are many factors that impact the outcome. Your doctor will discuss this with you based on your individual case and your preferences.
- In some cases, there is no fetal heartbeat present. This means the pregnancy is not viable and you have miscarried.
- Some women may choose to wait and see rather than have treatment. This means letting nature take its course.
- Usually, you will have bleeding vaginally, which may be similar to or heavier than a period.
- In some cases, the bleeding can be very heavy which means you may need surgery to remove the pregnancy or medical treatment to help you pass the pregnancy. This is similar to women who are having a miscarriage.
- Usually, your doctor will arrange for you to have another scan a few days or weeks afterwards. This is to make sure there is no pregnancy left inside the womb.
What are the risks for a future pregnancy after being diagnosed with a Caesarean scar pregnancy?
- The risk of having another CSP in a future pregnancy depends on the type of CSP and how it was managed.
- However, overall the risk of having another CSP may be quite high. Some medical studies have suggested this may be as high as 20-30% (1 in 5 to 1 in 3 women). However, as CSP is a rare complication of pregnancy, we are still in the process of learning more about this condition.
- Therefore, it is advised to have an early pregnancy scan at approximately 5-6 weeks (as soon as the missed period and/or a positive pregnancy test is apparent) in any future pregnancy, to rule out another CSP or make the diagnosis as early as possible.
Dr Helena Bartels, Dr Andrea Kaelin-Agten , Prof Ilan E. Timor-Tritsch, Dr Stephen Carroll, Ms Naomi Cooney, along with mums in Placenta Accreta Ireland.

